On February 11, the "Patient control" public organisation reported a sudden-onset shortage of antiretroviral treatment in the Saint Petersburg-based AIDS facility. Doctors there became concerned that the quantity of their ART supplies might not be enough to treat all the patients.
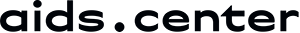
To confirm their own words, the activists used their Facebook page to published a copy of the order issued by the health care facility Chief Medical Officer, Denis Gusev.
As it follows from the order, now, to stretch out medical supplies, an amount of drugs such as etravirine (Intelence), dolutegravir (Tivicay), fosamprenavir (Telzir), and lamivudine/zidovudine will be distributed in the city on the Neva river, sufficient for one month only, along with other medications – for two months only (instead of three months).
The reason lies in the actions of the Ministry of Health of the Russian Federation, which procures medicine for the regions on a centralised basis. In 2019, the Ministry announced auctions for the drug procurement too late, only at the end of January. In case of a successful completion of the tender process, the supplying of medicine to the regions might start in April or May at best.
Organisations for patients are convinced that regional AIDS facilities might have run out of their medical supplies even before that, and will end up having no medicine for the treatment of their patients. Their concerns are shared among the regions.
A situation similar to the one in Saint Petersburg happened in Sevastopol. According to the website of the local TV channel NTS, five and a half million roubles from the reserve fund of the city budget will be spent on the urgent purchase of medicines.The city needs ART medications badly.

Meanwhile, as local officials claim, this emergency situation has occurred due to some technical difficulties that "the Ministry of Health of the Russian Federation had faced".
Following the media feeds, AIDS.CENTER has tried to figure out what the situation is like in other places. Here is the answer: It is poor. The shortage of medicine is not a local problem. It is a national one. For a country withover a million HIV-positive residents, the consequences of such technical difficulties can be fatal.
From Moscow to Siberia
"We have run out of medications as well," the HIV-positive woman from Tyumen says. She asked not to reveal her name. "Previously, I used to follow such an ART-plan: amiviren — tenofovirum — raltegravirum. Today, February 12, as usual, I went to get a new portion, but the doctor said that there was no raltegravir, and no further supplies are expected to come in the nearest future. He suggested to replace the drug with its alternatives. However, these have numerous side effects, and I have a small child. If [in the future] I become disabled, it can seriously affect my baby. "The previous treatment plan worked well for me in terms of tolerability, and I had an undetectable viral load".
The doctor did not explain why there were no drugs, but added that medications will be available around May at best.

Another person to whom we talked, also from Siberia, confirms her compatriot's words, and immediately brings up her own experience: "I used to take dolutegravir — amiviren — tenofovir, and now they gave me tenofovir — lamivudine — etravirine. Accordingly, this has increased the medication intake from once to twice a day".
An increased number of medication intake always affects a patient negatively. This parameter is considered to be critical in terms of adherence. It also equally increases the frequency of visits to the doctor.
'Previously, the medications were distributed in amounts sufficient for a three-month intake, and now for one month only. In reply to the question on how to proceed, the doctors suggested that we give them a call after February 20, and inquire - "maybe something will change"', this woman adds.
The situation with drug availability in Moscow is no better.
"During my visit to the city health center in Sokolinaya gora District, an infectious disease doctor suggested replacing Intelence (etravirine) with Elpida or Edurant (rilpivirine)," a man, who asked not to reveal his name, tells. "The doctor referred to the unavailability of the medication in the drug store".
To the question on the future availability of the drug this man had previously gotten, the reply was: "Check back in May, maybe". Just like their colleagues from Tyumen, doctors from Sokolinaya gora District are realistic about the time it might take to resolve the problem. It is not for the first time that they face a shortage of medication caused by the Ministry's actions, so they are fully aware of how slow the government machine works.
Procurement system
It has been three consecutive years that ART medications have been purchased on a centralised basis in Russia. In July 2016, Vladimir Putin, the President of the Russian Federation, passed the law authorising the switch from the regional model of ART public procurement system, to the centralised model, with the Ministry of Health being responsible.
This step enabled huge pharmaceutical companies to force small regional companies out of the market — they simply cannot supply the required amount of drugs on a federal level. Meanwhile, the purpose of this solution was to put an end to the "mess" of regional supplies, and, most importantly, to reduce the cost of medications.
"I used to take dolutegravir — amiviren — tenofovir, and now they gave me tenofovir — lamivudine — etravirine. Accordingly, this has increased the medication intake from once to twice a day".
The latter should have enabled the increase of therapy coverage, and the amount of pills purchased annually at government expense, with the same level of funding.
According to one of the leading pharmaceutical experts of the country, the Director of the Research Institution of Health Care and Medical Management, David Melik-Guseinov, within the previous procurement system, local authorities in many regions preferred to do business with only one supplier, that is, a local monopolist, which enabled it to dictate the pricing policy. His words were cited by the Kommersant newspaper.
Sergey Shulyak, the DSM Group Director and pharmaceutical analyst, also agreed with him. "Centralised procurement is simply cheaper. If procurement is carried out by each region separately, goods turn out to be procured in smaller amounts, but, respectively, at a higher price. Moreover, within the previous system, procurement was still funded by the federal budget, so it only made sense to move the spending authority to the federal level," this is what the expert said at that time in an interview held by the AIDS.CENTER correspondent.

Well, it did not take long to see the result of this reform: According to the data provided by DSM Group, the marketing agency specialising in pharmaceutical market research, the centralisation of ART procurement in 2017 has reduced the prices of some drugs by as much as 40%.
A little later, the government announced that starting from January 1, 2018, its specialists will adopt a new pricing methodology, in which, along with the analysis of prices offered by potential suppliers, congruous market and marginal prices for each drug will be compared. All these measures were supposed to enhance the efficiency of centralised procurement. However, unfortunately, the very opposite has happened.
"Positive" result
The purchase cost issue causes reasonable questions: Since 2006, there has been an average of 10-12% in annual increase in the number of new HIV incidents in the country. And in ten years, the ART coverage has grown almost sixfold.
"To prevent the virus from reproducing in the body, ART medication must be taken daily, for the rest of a life. The termination of the therapy not only means the return of symptoms, but could also cause the development of drug resistance."
Back in the day, Kommersant wrote that in 2018, the Ministry of Health managed to save up to one billion roubles on anti-HIV, hepatitis, and tuberculosis medications. (The Ministry spent 23,3 billion roubles on anti-HIV, hepatitis and tuberculosis medication procurement, while having signed 100 contracts; in 2017, with comparable amounts, it signed 122 contracts, for a total of 24,6 billion roubles.
However, according to the analysis of the "Treatment Preparedness Coalition", nowadays, the anti-HIV medication procurement amount in our country might be reduced. Thus, experts believe that in 2019, the patients could have been short of three thousand ART courses.
Moreover, the governmental centralised procurement system regularly facesinterruptions in the supply of ART medications.
Only in 2018, such cases happened in The Republic of Bashkortostan, Altai Krai, Kaliningrad Oblast, Crimea, Novgorod, and in prison camps of Sverdlovsk Oblast and Krasnoyarsk.
As previously stated by activists and pharmaceutical experts, the problem with delays is a systemic one, and is associated with the fact that the budget was adopted by the government in December. This implies that the Ministry usually announces its first auctions only in the last week of February, and that it starts the procurement process only in March. And every year it is the same.
Market rules
"The pharmaceutical business is a market of which we need to have a clear understanding of the amount of goods necessary, and the appropriate time to supply them," says Nikolay Bespalov, the RNC Pharma Development Director on the procurement system for AIDS.CENTER in October. And this is the key point.
on the topic
Treatment
Withdrawal syndrome. How did Crimea end up without methadone?
Due to late planning, a supplier launches negotiations with the manufacturer only after it has won the auction, to minimise the risks. As a result, manufactures cannot meet the deadlines, and often delay shipments. (This is exactly the way R-Pharm, for instance, explains the interruptions in supplies of some pharmaceuticals, which AIDS.CENTER has repeatedly covered in its reports).
The manufacturing plant has just a couple of months to dispatch the annual amount of medicine, while the amounts in stock are usually insufficient, because the manufacturer does not store amounts exceeding the quantity it will manage to sell on its own, without the government contract.
In the end, no one from the chain — neither the government, nor the firms producing medicine, or intermediary companies — seems eager to take obvious, commercial risks, with all of them shifting responsibility to the patient. And all that results in the unexplainable changes in treatment plans, and the absence of required medicine in stock.
As of mid February, 2019, the Ministry has not yet signed any contracts. They have announced only a small part of the schedule, but even here everything depends on a distributor: whether it would want to supply everything at once, or would rather delay supplies up to the date that is specified in the contract," Alexey Mikhailov, Head of the ITPCru (Treatment Preparedness Coalition) Monitoring Department, comments on the current situation.
"However," he remarks, "this year, when the issue with the supplies, and the shortage of medicine became especially acute, the Ministry of Health announced the first auctions one month earlier compared to 2018, which means that there is a chance to avoid a disaster".
Sticking to the formula
Everybody knows that ART is considered successful, when the number of copies per one microlitre of a patient's blood is reduced down to less than 50. Such a viral load is called "undetectable". This is an important medical and preventive parameter. A patient with an undetectable viral load cannot transmit the virus to a partner, even through unprotected sex.
"As a result nobody from the chain — neither the government, nor firms releasing medicine, or intermediary companies — wants to take obvious, commercial risks, and everyone shifts responsibility to a patient."
The amount of CD4-lymphocytes of a patient with such a viral load usually increases up to 500 cells per millilitre, which protects them from the associated diseases that cause lethal outcomes among AIDS-positive people. If before a treatment, any symptoms of these diseases had been in place, this would be the exact moment when all of them disappear, and an HIV-positive person's life, in most respects, becomes almost similar to that of a healthy person.
However, to prevent the reproduction of the virus in the body, ART medicines should be taken daily, for the rest of a life. The break of the therapy not only means an increase of the viral load and automatic return of symptoms, but could also cause the development of resistance to the medicine that a patient had been receiving before interruptions began or a therapy was terminated.

It is considered that the epidemic can be stopped only by reaching the figures known as "formula 90 — 90 — 90". According to this formula, 90% of the HIV-positive must be aware of their diagnoses; 90% of those aware must get treatment; 90% of those who get treatment must have the viral load lowered to the undetectable level.
It is obvious that breaks make for the possibility to achieve this result (and Russia, as many other countries, took the responsibility to reach it by 2020) equal to zero.
Regional question
According to Yulia Vereschagina, project Pereboi.ru Consultant, apart from the regions already mentioned in the media, this February, the following regions have already faced a shortage of medicine: Nizhny Novgorod Oblast, Rostov Oblast, Crimea, Federal Penitentiary Service of Perm Krai, Samara Oblast, and Saint Petersburg. Interruptions of diagnostic means availability are in place in the Republic of Bashkortostan, Dagestan, and Ryazan Oblast.
on the topic
Prevention
How the only HIV NPO in the Orenburg region is fighting the epidemic
With one remark: A female activist asks not to include Saint Petersburg in their list: "In Saint Petersburg, the amount of pills we get at once has been reduced, but the treatment plans remain unchanged. This is a common practice before new portions are supplied, and almost everyone does it, though in Saint Petersburg, our medical authorities officially make it public," she clarifies. "It's frustrating, but we do not consider it an interruption".
Alexey Lakhov, staff member of Humanitarian action, one of the main city AIDS-service organisations that were requested by AIDS.CENTER to comment on the situation, also agrees that there is no need to dramatise: "There are no such problems, we've simply started providing medicine for shorter periods, but the situation is under control".
Most experts agree that the current situation could be prevented by virtue of long-term contracts to make manufacturers and distributors aware of the anticipated contract amounts in advance, and keep government procurement schedules stable. "Nothing prevents the government from concluding one contract for several years, abandoning annual launch of the procedure," they believe.
"I think there is no need to go back to the decentralised or regional procurement systems, since the regions have already shown that not everyone can manage it, with some regions doing well, and others very poorly, and it will also increase the prices again," Alexey Mikhailov, Head of the ITPCru Monitoring Department, concludes. "Here's my opinion: We need to switch to the long-term contracts, which will allow for the reduction of prices, and prevent interruptions at least for several years, provided, of course, that the healthcare funding is increased".